Considerations for use of QUVIVIQ™

Considerations for use of QUVIVIQ™
Bunmi would be a suitable candidate for QUVIVIQ™
Indication11
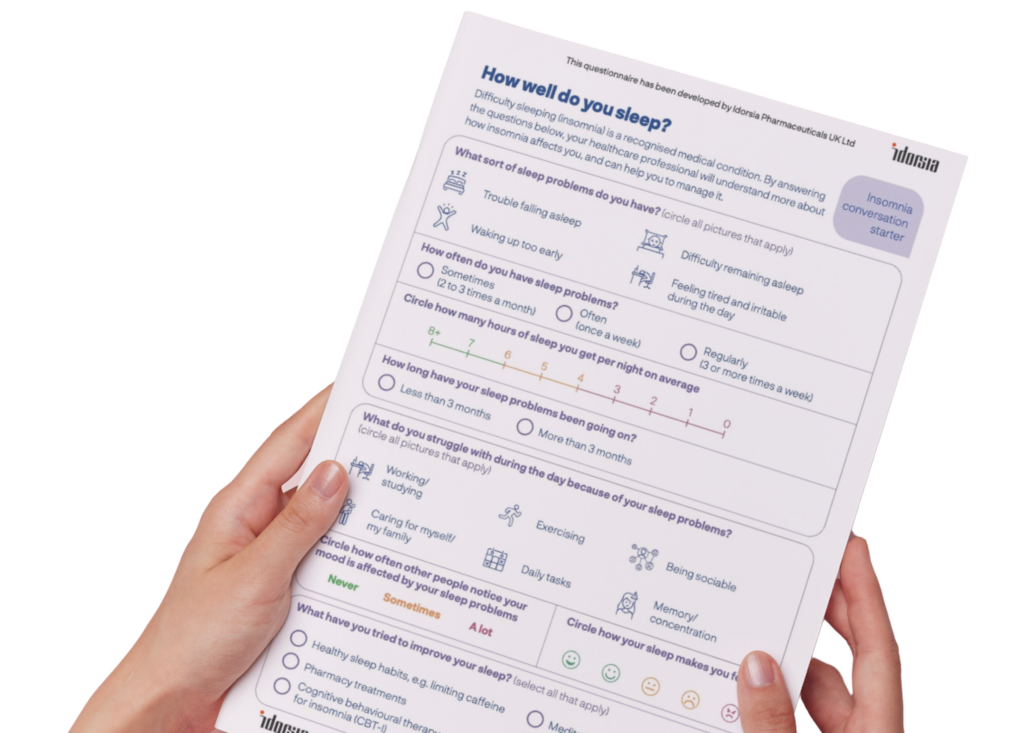
QUVIVIQ™ (daridorexant) is indicated for the treatment of adult patients with insomnia characterised by symptoms present for at least 3 months and considerable impact on daytime functioning.
Bunmi meets the licence criteria
NICE12
Daridorexant [QUVIVIQ™] is recommended for treating insomnia in adults with symptoms lasting for 3 nights or more per week for at least 3 months, and whose daytime functioning is considerably affected, only if:
- cognitive behavioural therapy for insomnia (CBTi) has been tried but not worked, or
- CBTi is not available or is unsuitable
Driving11
Because QUVIVIQ™ acts by reducing wakefulness, patients should be cautioned about engaging in potentially hazardous activities, driving, or operating heavy machinery unless they feel fully alert, especially in the first few days of treatment.
Propensity for dependence
Bunmi says she is concerned about the addictive properties of ‘sleeping tablets’.
- Dual orexin receptor antagonists (DORAs) such as QUVIVIQ™ appear to be non‑habit‑forming, hence their suitability for longer‑term use13
- There was no evidence of abuse or withdrawal symptoms indicative of physical dependence when QUVIVIQ™ treatment was discontinued after 12 months in clinical trials11
- DORAs block the wake-promoting action of orexin - promoting sleep but without any widespread inhibition of the CNS11,14,15
- Traditional hypnotic or sedative drugs, by contrast, drive sleep by broad suppression of the CNS; along with a number of side effects, there is a risk of dependence and tolerance15
Benefit/ risk profile
Bunmi’s GP explains that the most common adverse reactions seen with QUVIVIQ™ are headache and somnolence. Other common side effects include dizziness, nausea and fatigue. Sleep paralysis, hallucinations, somnambulism (sleepwalking), abnormal dreams/nightmares and hypersensitivity have also been reported; she asks Bunmi to contact her if she experiences any of these.11
Bunmi’s GP, after discussing the potential benefits and risks with her, elects to prescribe QUVIVIQ™ – a 50 mg dose to be taken on a nightly basis, 30 minutes before going to bed.11*
- If a patient forgets to take QUVIVIQ™ at bedtime, that dose should not be taken during the night.
- QUVIVIQ™ can be taken with or without food. However, taking it soon after a large meal may reduce the effect on sleep onset.
She arranges another appointment in 5 weeks to assess Bunmi’s response. Treatment with QUVIVIQ™ should be as short as possible, and appropriateness of continued treatment should be assessed within 3 months and regularly thereafter.11,12
*Based on clinical judgement, some patients may be treated with 25 mg QUVIVIQ™ once per night. The recommended dose for patients with moderate hepatic impairment or who are taking concomitant moderate CYP3A4 inhibitors is 25 mg once per night.11 Consult the Summary of Product Characteristics for complete prescribing information.
Ready for the next step?
Medication follow-up appointment 1 (5 weeks later)
CBT: cognitive behavioural therapy; CBTi: cognitive behavioural therapy for insomnia; CNS: central nervous system; DORA: dual orexin receptor antagonists; HRT: hormone replacement therapy; NICE: National Institute for Health and Care Excellence; OTC: over-the-counter; PRO: patient-reported outcome
QUVIVIQ™ is indicated for the treatment of adult patients with insomnia characterised by symptoms present for at least 3 months and considerable impact on daytime functioning.21
This information is intended for UK healthcare professionals.
Adverse events must be reported. Healthcare professionals are asked to report any suspected adverse reactions via www.mhra.gov.uk/yellowcard or search for MHRA Yellow Card in Google Play or Apple App Store. Adverse events should also be reported to ds.safety.uk@idorsia.com
References
- The Epworth Sleepiness Scale. Available at: nasemso.org. Accessed August 2025
- Riemann D, Espie C A et al. The European Insomnia Guideline: an update on the diagnosis and treatment of insomnia 2023. J Sleep Res 2023;32(6):e14035
- Stern A F. The hospital anxiety and depression scale. Occup Med (Lond) 2014;64(5):393-394
- World Health Organization (WHO). International statistical classification of diseases and related health problems (ICD) 11th revision. Available at: icd.who.int. Accessed August 2025
- National Institute for Health and Care Excellence (NICE). Clinical knowledge summary. Insomnia. Scenario: managing long-term insomnia (more than 3 months duration), May 2025. Available at: cks.nice.org.uk. Accessed August 2025
- Riemann D, Baglioni C et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res 2017;26(6):675-700
- Koffel E, Bramoweth A D, Ulmer C S. Increasing access to and utilization of cognitive behavioral therapy for insomnia (CBT-I): a narrative review. J Gen Intern Med 2018;33(6):955-962
- Morin C M, Belleville G et al. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 2011;34(5):601-608
- National Institute for Health and Care Excellence (NICE). Clinical knowledge summary. Insomnia. Prescribing information: Z-drugs, May 2025. Available at: cks.nice.org.uk. Accessed August 2025
- Prolonged-release melatonin Summary of Product Characteristics
- QUVIVIQ™ Idorsia Pharmaceuticals Ltd, Summary of Product Characteristics
- National Institute for Health and Care Excellence (NICE). Technology appraisal guidance 922. Daridorexant for treating long-term insomnia, 18 October 2023. Available at: nice.org.uk. Accessed August 2025
- Muehlan C, Roch C et al. The orexin story and orexin receptor antagonists for the treatment of insomnia. J Sleep Res 2023;32(6):e13902
- Janto K, Prichard J R, Pusalavidyasagar S. An update on dual orexin receptor antagonists and their potential role in insomnia therapeutics. J Clin Sleep Med 2018;14(8):1399-1408
- Roch C, Bergamini G et al. Nonclinical pharmacology of daridorexant: a new dual orexin receptor antagonist for the treatment of insomnia. Psychopharmacology (Berl) 2021;238(10):2693-2708
- National Institute for Health and Care Excellence (NICE). Clinical knowledge summary. Benzodiazepine and z-drug withdrawal. Scenario: benzodiazepine and z-drug withdrawal, May 2025. Available at: cks.nice.org.uk. Accessed August 2025
- National Institute for Health and Care Excellence (NICE). Clinical knowledge summary. Benzodiazepine and z-drug withdrawal. Prognosis, May 2025. Available at: cks.nice.org.uk. Accessed August 2025
- Mignot E, Mayleben D et al. Safety and efficacy of daridorexant in patients with insomnia disorder: results from two multicentre, randomised, double-blind, placebo-controlled, phase 3 trials. Lancet Neurol 2022;21(2):125-139
© NICE 2023 Daridorexant for treating long-term insomnia. Available from www.nice.org.uk/guidance/ta922. All rights reserved. Subject to Notice of rights.
NICE guidance is prepared for the National Health Service in England. All NICE guidance is subject to regular review and may be updated or withdrawn. NICE accepts no responsibility for the use of its content in this product/ publication.
UK-DA-00657 | Date of preparation: September 2025